
New Publication: Bicuspid Aortic Valve & Aneurysm Repair
Early Results for Bicuspid Aortic Valve Repair during Aortic Aneurysm Surgery: Multi-Institutional Analysis
Bicuspid Aortic Valve Repair with the HAART 200 Aortic Annuloplasty Devices
- 127 Patients from 27 Centers
- Proximal Aortic Aneurysm & BAV Repair with HAART 200
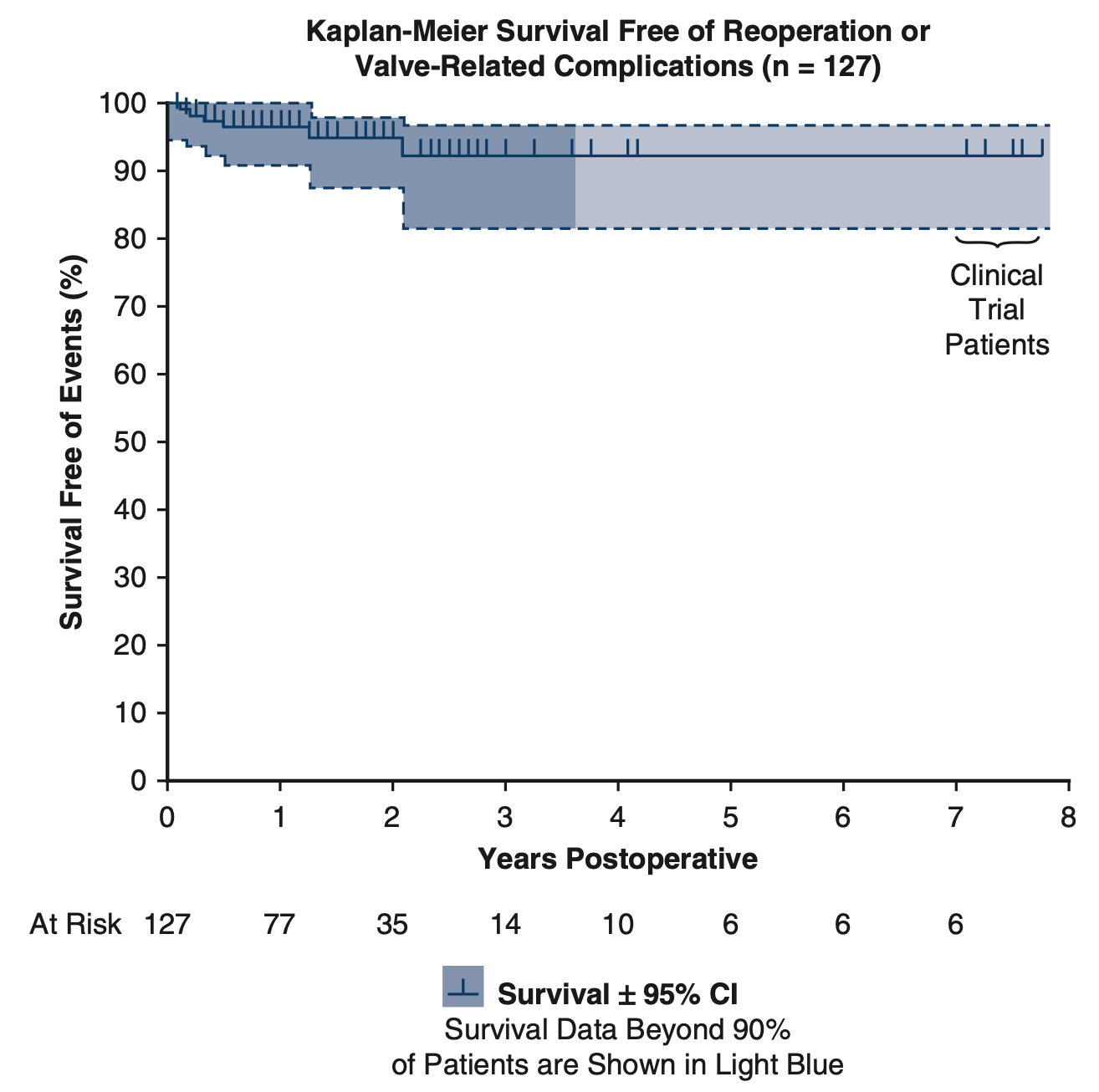
- Maximal Followup 7.7 years (mean 20 months)
- >90% Survival & Freedom from Valve-Related Complications
Central Message
Using bicuspid ring annuloplasty, leaflet reconstruction, and aortic root remodeling, most types of bicuspid valve defects associated with proximal aortic aneurysms can be repaired with good early results.
Perspective Statement
Routine bicuspid valve repair during aortic aneurysm surgery has been difficult for a variety of reasons. Bicuspid ring annuloplasty produces major annular remodeling and equalizes fused and non-fused segmental annular circumferences, facilitating leaflet reconstruction. Together with ascending aortic and selective sinus replacement, bicuspid valve repair can become routine with good early results.
Abstract
Objectives: Geometric ring annuloplasty has shown promise during bicuspid aortic valve (BAV) repair for aortic insufficiency (AI). This study examined early outcomes of BAV repair associated with proximal aortic aneurysm replacement.
Methods: From September 2017 to November, 2021, 127 patients underwent BAV repair with concomitant proximal aneurysm reconstruction. Patient age was 50.6±12.7 years (mean±SD), male gender was 83%, NYHA Class was 2 (1,2) (median[IQR]), and preoperative AI grade was 3(2,4). Ascending aortic diameter was 50(46,54) mm, and all patients had ascending aortic replacement. Forty had sinus diameters >45 mm prompting remodeling root procedures. One Hundred-five had Sievers Type 1 valves, 3 had Type 0, and 7 Type 2. One Hundred-eighteen had primarily right/left fusion, 8 had right/non fusion, and 1 left/non fusion. Leaflet reconstruction utilized central leaflet plication and cleft closure, with limited ultrasonic decalcification in 31.
Results: Ring size was 23(21,23) mm, and 26 of 40 root procedures were selective non-fused sinus replacements. Aortic clamp time was 139(112,170) minutes, and bypass time 178(138.217) minutes. Post-repair AI grade was 0(0,0) (p<0.0001), and mean valve gradient was 10(7,14) mmHg. No early, and one late mortality occurred. Four patients required reoperation for bleeding, and 4 needed pacemakers. At a mean follow-up of 20 months (maximal 93), there were no valve-related complications, 5 late repair failures prompting valve replacement, and 1 death from Covid.
Conclusions: Geometric ring annuloplasty for BAV repair with proximal aortic aneurysm reconstruction is safe and associated with good early outcomes. Further experience and followup will help inform long-term durability.
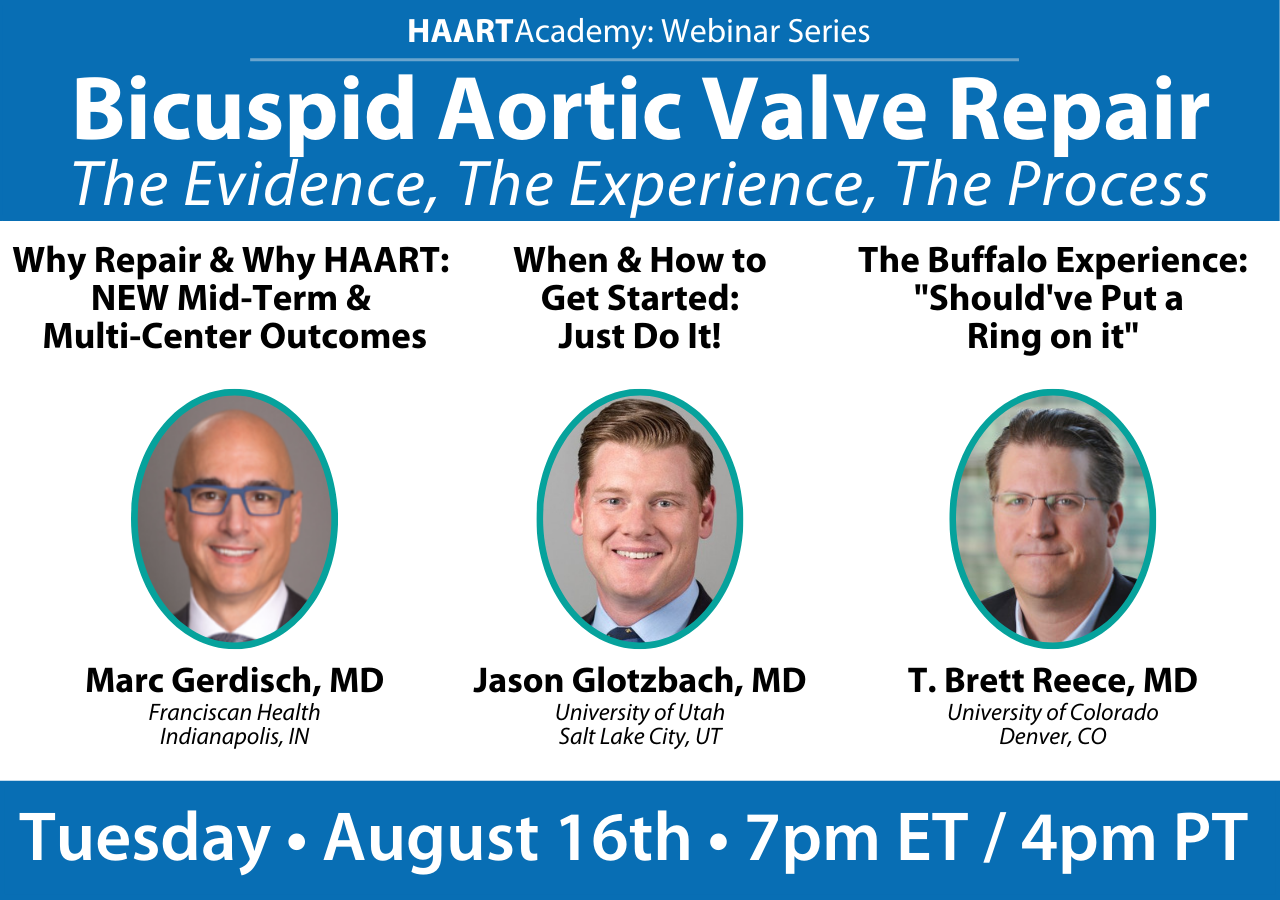
Register for the next
HAART Academy Webinar
August 16th - 7 pm ET / 4 pm PT
Busy at the scheduled time? Register and you will recieve a recording after the event. Learn more
Current technique of BAV repair to optimize late success rates
Theodor J. M. Fischlein MD, Vinay Badhwar MD, J. Scott Rankin MD
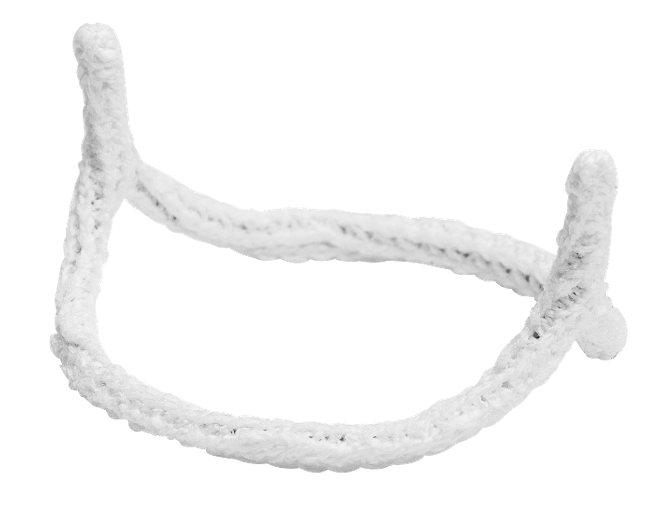
HAART 200 Aortic Annuloplasty Devices
Simplifying and Standardizing Bicupid Aortic Valve Repair
- Symmetric 180-degree valve repair
- No-deep root dissection or coronary reimplantation required
Bicuspid Aortic Valve Repair with Associated Semi-Root Remodeling
Dominic Emerson MD, Alfredo Trento, MD, J. Scott Rankin MD, Vinay Badhwar MD & Joanna Chikwe MD
1,500+
Devices Placed
150+
Trained Surgeons
40+
Peer-reviewed Publications
Learn More
Send me more information on the HAART Aortic Annuloplasty Devices

Simplifying & Standardizing Aortic Valve Repair
- Resize - Reduce Dilatation
- Reshape - Restore more normal, three-dimensional coaptation geometry
- Stabilize - Reduce the risk of recurrent annular dilatation